
Compliance with the Health Insurance Portability and Accountability Act is more than just a legal obligation; it's an important step toward preserving patients' trust and privacy. To assist healthcare providers in achieving HIPAA compliance in 2023, we have created this comprehensive checklist. Let's dive into the details.
Understanding HIPAA Compliance
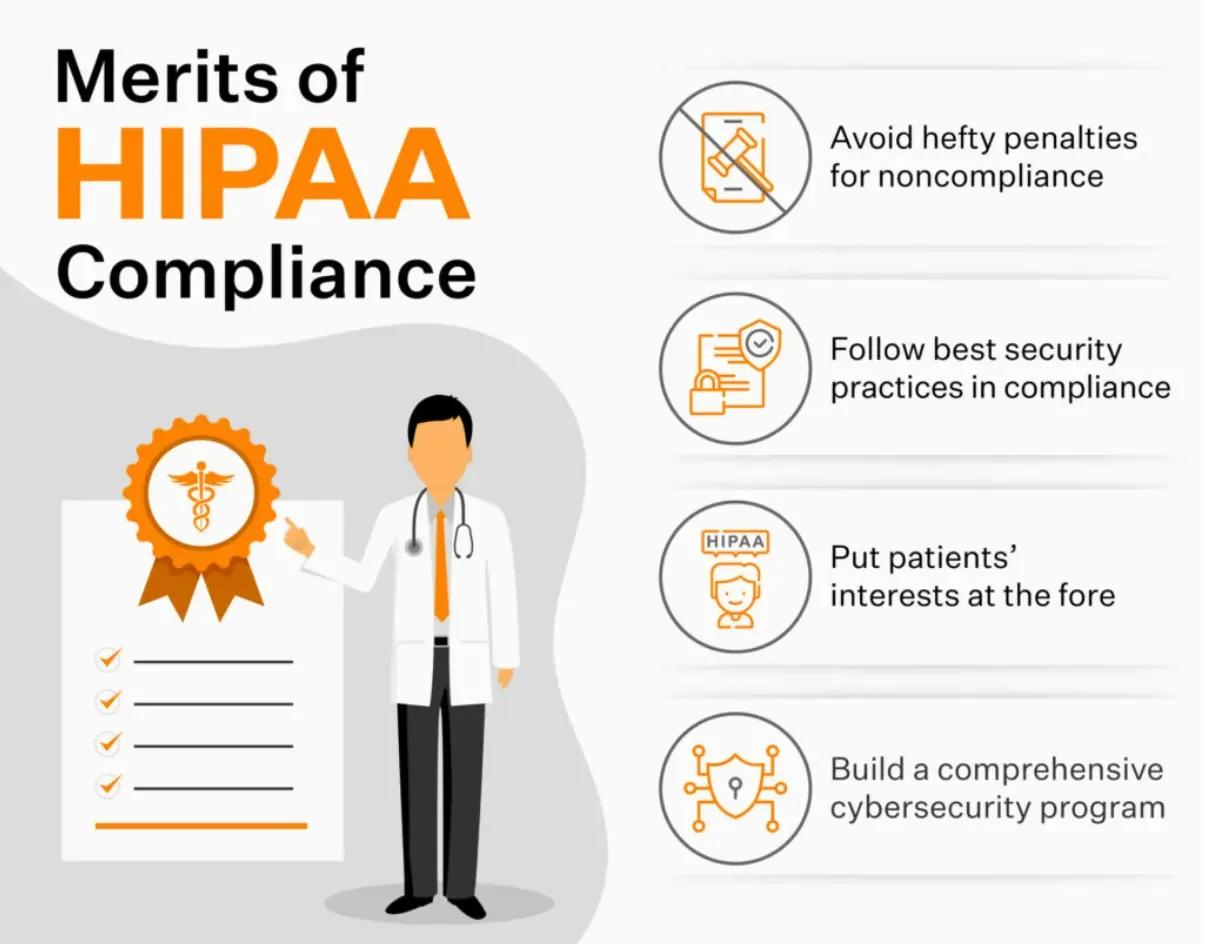
The HIPAA Act was enacted by federal law in 1996 requiring the protection and security of personal health information. For the covered entities, such as healthcare providers, health insurance companies, and medical information clearinghouses, compliance with HIPAA is necessary. Sanctions and reputational damage can be imposed in the event of failure to comply. The following essential areas should be addressed by the organizations in order to guarantee compliance:
1. Administrative Safeguards
Implementing Policies and Procedures: Develop and enforce comprehensive policies and procedures to address all aspects of compliance with the Health Insurance Portability and Accountability Act. Guidelines for access to data, disclosure, and training of workers as well as an incident response should be included.
Appointing a Privacy Officer: Designate a privacy officer responsible for overseeing and managing HIPAA compliance efforts within the organization. The Privacy Officer should ensure that policies are in place, audits are carried out regularly and privacy questions are dealt with.
Performing Risk Assessments: To identify possible vulnerabilities and to put in place measures to mitigate risks, perform regular risk assessments. In this context, physical, technical, and administrative safeguards as well as any security weaknesses should be assessed and addressed.
2. Physical Safeguards
Securing Facilities: Implement physical security measures, such as access controls, video surveillance, and visitor logs, to protect physical areas where patient information is stored or accessed.
Workstation Security: Ensure workstations are secure by implementing policies that require employees to log out or lock their computers when not in use. Encryption and strong passwords should be used to protect data stored on workstations.

3. Technical Safeguards
Access Control: Implement secure user authentication mechanisms, such as unique usernames and strong passwords, to control access to electronically protected health information (ePHI). Regularly review and update user access privileges based on employees' roles and responsibilities.
Encryption and Data Protection: Implement encryption technology to protect ePHI both in transit and at rest. This helps ensure that even if data is intercepted or stolen, it remains unreadable and unusable to unauthorized individuals.
Regular System Updates and Patches: Keep all software and systems up to date with the latest security patches and updates. This helps protect against known vulnerabilities and reduces the risk of unauthorized access or data breaches.
4. Training and Awareness
Employee Training: Provide comprehensive HIPAA training to all employees who handle patient data. This training should cover the importance of patient privacy, security best practices, and how to handle and report potential security incidents.
Ongoing Awareness Programs: Foster a culture of security awareness within the organization by conducting regular training sessions, sending out security reminders, and promoting best practices through internal communications channels.
5. Business Associate Agreements
Identifying Business Associates: Identify and enter into written agreements with business associates who have access to patient information. Business associate agreements outline their responsibilities and ensure they comply with HIPAA regulations.
Due Diligence: Conduct due diligence when engaging with business associates to ensure they have appropriate safeguards in place to protect patient information. Regularly review and update these agreements to reflect any changes in the business relationship.
6. Incident Response and Breach Notification
Developing an Incident Response Plan: Create a comprehensive incident response plan that outlines the steps to be taken in the event of a security incident or data breach. This plan should include procedures for reporting, investigating, and mitigating incidents, as well as guidelines for notifying affected individuals and regulatory authorities.
Testing and Reviewing the Plan: Regularly test and review the incident response plan to ensure its effectiveness. Conduct simulated exercises and tabletop drills to identify any gaps or weaknesses in the plan and make necessary improvements.
Breach Notification: Familiarize yourself with the breach notification requirements outlined in the HIPAA regulations. In the event of a breach, promptly assess the situation, determine the scope of the breach, and notify affected individuals, the Department of Health and Human Services (HHS), and other relevant parties as required.
7. Documentation and Record-Keeping
Maintaining HIPAA Policies and Procedures: Keep detailed documentation of all policies, procedures, and activities related to the HIPAA compliance checklist. This documentation should include records of risk assessments, training sessions, incident response actions, and business associate agreements.
Retention of Records: Follow the recommended retention periods for HIPAA-related records, including policies, training records, incident response documentation, and business associate agreements. Retaining records for the required timeframe ensures compliance and facilitates audits and reviews.
Conclusion
HIPAA compliance is a vital aspect of healthcare operations, ensuring the protection of sensitive patient information. By implementing the administrative, physical, and technical safeguards discussed in this comprehensive checklist, healthcare organizations can establish a robust compliance framework. Regular training, awareness programs, and incident response planning are crucial for maintaining HIPAA compliance in an evolving threat landscape. Remember to document all compliance efforts and regularly review and update your policies and procedures to stay current with regulatory requirements. By prioritizing HIPAA compliance, healthcare organizations can safeguard patient privacy, maintain trust, and avoid costly penalties.
FAQs
Q1: What is the purpose of HIPAA compliance?
HIPAA compliance ensures the protection, security, and confidentiality of individuals' health information, promoting patient privacy and trust while providing guidelines for healthcare organizations to follow.
Q2: Who needs to comply with HIPAA regulations?
Covered entities, including healthcare providers, health plans, and healthcare clearinghouses, must comply with HIPAA regulations. Business associates who have access to patient information are also required to comply.
Q3: What are some consequences of non-compliance with HIPAA regulations?
Non-compliance with HIPAA regulations can result in significant penalties, ranging from fines to criminal charges, depending on the severity of the violation. Additionally, organizations may face reputational damage and loss of patient trust.